Table of Contents
Introduction: Lifestyle Diseases and Global Health Turning Point
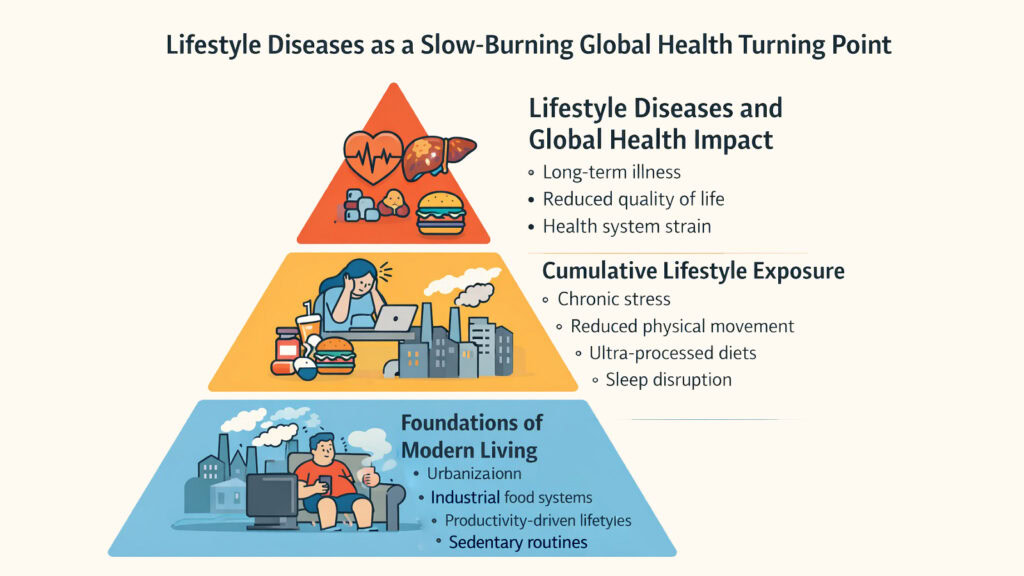
The world faces a strange paradox. Medical science has conquered many infectious diseases that once decimated populations. Yet now, in an era of unprecedented comfort and technological advancement, humanity confronts a new category of killers. These are not diseases born from viruses or bacteria. They emerge from the way people live, work, eat, and move through their days. Lifestyle diseases have become the defining health challenge of the modern world, quietly reshaping mortality patterns across every continent.
These conditions develop slowly, almost invisibly. They accumulate over years of small choices and environmental exposures. A desk job here, processed meals there, shortened sleep cycles, constant digital engagement. Each element seems harmless in isolation. Together, they form a pattern that overwhelms the body’s adaptive capacity. By the time symptoms appear, damage has often progressed beyond easy reversal. The liver shows fatty deposits. Arteries narrow. Blood sugar regulation fails. Mental resilience erodes.
What makes lifestyle diseases particularly dangerous is their systemic nature. They do not strike randomly. They follow the contours of modern urban design, food systems, work cultures, and social structures. Cities are built for cars rather than walking. Food industries are optimized for shelf life rather than nutrition. Workplaces that demand constant availability. Social environments that replace face-to-face connections with screen-mediated interaction. These are not individual failings but environmental realities that shape health outcomes on a massive scale.
The eight lifestyle diseases examined in this article represent the most significant threats to global health today. Type 2 diabetes, cardiovascular disorders, obesity, hypertension, chronic respiratory conditions, fatty liver disease, mental health disorders, and certain cancers share a common origin. They emerge from abundance rather than scarcity, from comfort rather than hardship, from speed rather than rest. Understanding them requires looking beyond individual pathology to examine how societies structure daily life itself.
Global Impact of Major Lifestyle Diseases
| Lifestyle Disease | Global Health Impact |
|---|---|
| Type 2 Diabetes | Affects over 530 million adults worldwide, projected to reach 640 million by 2030 |
| Cardiovascular Diseases | Leading cause of death globally, accounting for approximately 32% of all deaths |
| Obesity | Global prevalence has nearly tripled since 1975, affecting over 650 million adults |
| Hypertension | Affects 1.28 billion adults aged 30-79 years worldwide, often undiagnosed |
| Chronic Respiratory Diseases | Responsible for 4 million deaths annually, third leading cause of death globally |
| Non-Alcoholic Fatty Liver Disease | Affects approximately 25% of global population, rising rapidly in developed nations |
| Depression and Anxiety Disorders | Over 280 million people affected by depression, 301 million by anxiety disorders |
| Lifestyle-Linked Cancers | Approximately 30-50% of cancer cases linked to modifiable lifestyle factors |
1. Lifestyle Diseases and Type 2 Diabetes: The Cost of Abundance
For most of human history, diabetes was rare. The human body evolved to manage periods of scarcity, storing energy efficiently against uncertain food supplies. But modern life has inverted this equation entirely. Now the challenge is not finding calories but escaping them. They appear in vending machines, convenience stores, drive-throughs, and office break rooms. The body’s ancient mechanisms, designed for occasional abundance, face constant surplus. This mismatch lies at the heart of Type 2 diabetes as a lifestyle disease.
Sedentary work patterns have become the norm rather than the exception. Office workers sit for eight to ten hours daily. Commutes happen in cars or trains, not on foot. Entertainment unfolds on screens. Physical activity, once woven into daily survival, has become optional, something scheduled if time permits. Meanwhile, the food environment has shifted dramatically. Ultra-processed foods dominate supermarket shelves. These products are engineered for palatability and profit, loaded with refined sugars, unhealthy fats, and empty calories. They provide energy without nutrition, satisfaction without satiety.
The metabolic consequences unfold gradually. Insulin, the hormone that regulates blood sugar, must work harder and harder to process the constant glucose influx. Muscle cells, which normally absorb glucose during activity, remain inactive. Fat tissue accumulates, particularly around internal organs, creating inflammation that further disrupts insulin signaling. Over the years, this chronic overload exhausts the pancreas. Beta cells that produce insulin begin to fail. Blood sugar levels rise. Damage spreads to blood vessels, nerves, kidneys, and eyes.
What makes Type 2 diabetes particularly insidious among lifestyle diseases is its silent progression. People may live with prediabetes for years without knowing. No pain signals the gradual metabolic shift. By the time diagnosis occurs, complications may have already begun. Cardiovascular disease risk has multiplied. Kidney function has declined. Nerve damage has started. The disease represents not a sudden breakdown but the predictable outcome of a lifestyle design that prioritizes convenience over health.
Key Factors Contributing to Type 2 Diabetes as a Lifestyle Disease
| Factor | Impact on Diabetes Risk |
|---|---|
| Sedentary Behavior | Reduces insulin sensitivity by 40% compared to active individuals |
| Ultra-Processed Foods | Increase diabetes risk by 15% for every 10% increase in diet share |
| Added Sugar Consumption | Daily intake above 25g increases risk by 18% over time |
| Obesity | Increases diabetes risk 7-fold compared to normal weight individuals |
| Sleep Deprivation | Less than 6 hours nightly increases diabetes risk by 28% |
| Chronic Stress | Elevates cortisol, promoting insulin resistance and fat storage |
| Physical Inactivity | Less than 150 minutes weekly exercise doubles diabetes risk |
| Refined Carbohydrates | Cause rapid glucose spikes, exhausting insulin response mechanisms |
2. Lifestyle Diseases and Cardiovascular Disorders: Stress as a Daily Trigger
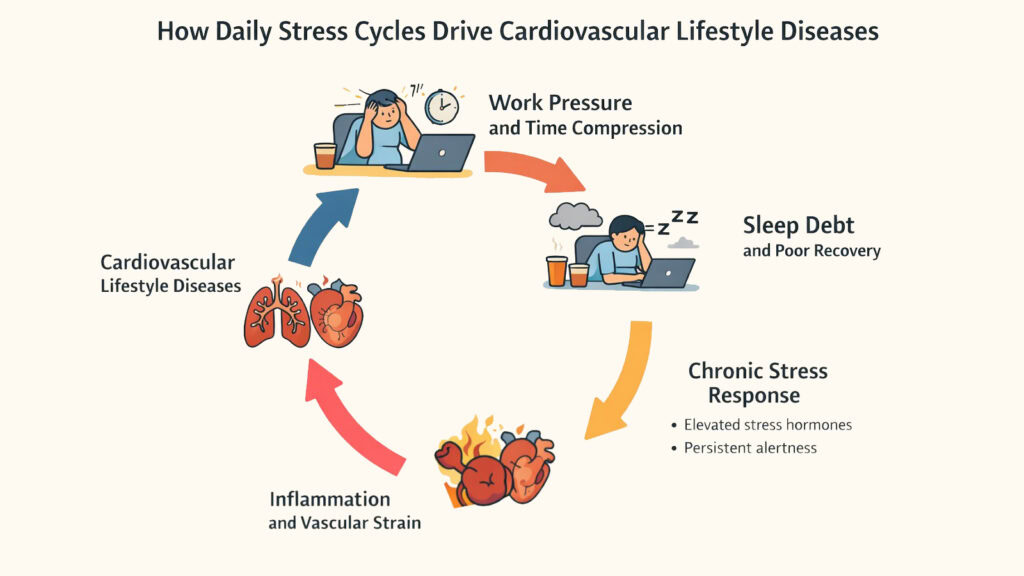
The heart was not designed for permanent urgency. Yet modern work culture operates in a state of constant activation. Deadlines pile up. Emails arrive at all hours. Performance metrics track every moment. The boundary between work and personal life has dissolved, leaving many people in a state of perpetual readiness. This chronic stress represents one of the most underappreciated drivers of cardiovascular disease, making it one of the most dangerous lifestyle diseases affecting global populations.
When the body perceives a threat, it mobilizes resources. Heart rate increases. Blood pressure rises. Stress hormones flood the system. This response evolved for brief physical dangers, not sustained psychological pressure. But in modern life, the threats are abstract and endless. Financial worries. Career uncertainty. Social comparison. Information overload. The stress response that should switch off remains chronically activated. This has profound cardiovascular consequences.
Chronic stress triggers inflammation throughout the cardiovascular system. Blood vessel walls become damaged and stiff. Cholesterol deposits form more easily in injured areas. Blood pressure stays elevated, forcing the heart to work harder with every beat. Sleep debt compounds the problem. Many people sacrifice rest to meet demands, unaware that sleep deprivation independently increases heart disease risk. During deep sleep, blood pressure normally drops, giving the cardiovascular system a chance to recover. Without adequate sleep, this recovery never happens.
The modern work environment has compressed life into smaller and smaller windows. People rush from task to task, eating quickly or skipping meals, moving less, sitting more. The concept of recovery time has nearly disappeared. Weekends fill with obligations. Vacations involve checking work messages. The heart, like any muscle, needs periods of lower intensity to maintain health. Without them, cumulative wear accelerates. Lifestyle diseases like cardiovascular disorders do not announce themselves with early warnings. They develop silently until a heart attack or stroke forces recognition.
Modern Lifestyle Factors Driving Cardiovascular Disease
| Factor | Cardiovascular Impact |
|---|---|
| Chronic Work Stress | Increases heart disease risk by 40% through sustained cortisol elevation |
| Sleep Debt | Less than 6 hours nightly raises cardiovascular mortality by 48% |
| Long Work Hours | Working over 55 hours weekly increases stroke risk by 35% |
| Social Isolation | Comparable cardiovascular risk to smoking 15 cigarettes daily |
| Sedentary Lifestyle | Each additional hour of sitting increases heart disease risk by 5% |
| Poor Diet Quality | Western diet patterns double cardiovascular disease incidence |
| Emotional Strain | Depression increases cardiac event risk by 60-80% over time |
| Lack of Recovery | Insufficient rest prevents cardiovascular repair and adaptation |
3. Lifestyle Diseases and Obesity: An Environmental Health Failure
Obesity has long been framed as a personal failing, a matter of insufficient willpower or poor choices. This perspective misses the larger truth. Obesity is an environmental disease, one of the most visible lifestyle diseases shaped by forces far beyond individual control. The modern environment consistently promotes energy intake while discouraging energy expenditure. This is not an accident but a design, the outcome of urban planning, food industry practices, and technological development that prioritize convenience and profit over health.
Consider the built environment. Cities sprawl outward, making car ownership necessary rather than optional. Sidewalks disappear or become discontinuous. Public transportation remains underfunded. Parks and green spaces shrink as development expands. The result is a landscape that makes physical activity difficult and driving easy. People do not choose sedentary lives so much as inherit them from infrastructure decisions made decades earlier. This environmental reality affects everyone but impacts lower-income communities disproportionately, where walkable spaces and recreational facilities are often scarce.
The food system compounds the problem. Ultra-processed foods dominate because they are cheap, convenient, and heavily marketed. Fresh produce costs more and spoils quickly. Cooking from scratch requires time that many people do not have. Fast food outlets cluster in certain neighborhoods, creating food environments where healthy choices are structurally limited. Meanwhile, portion sizes have expanded dramatically. What counted as a large serving thirty years ago is now standard or even small. People eating normal portions by current standards consume far more calories than previous generations.
Screen-based entertainment has replaced physical recreation for many, especially children. Video games, streaming services, and social media provide immediate gratification without requiring movement. The human body, evolved for constant motion, now sits for most waking hours. This shift happened within a single generation, too fast for biological adaptation. Obesity emerges from this mismatch, a predictable response to an environment of constant availability and minimal requirement for physical effort. Among lifestyle diseases, obesity stands out for how clearly it reflects systemic rather than individual failures.
Environmental Drivers of Obesity as a Lifestyle Disease
| Environmental Factor | Contribution to Obesity |
|---|---|
| Food Marketing | Children see 4,700+ food ads annually, 98% for unhealthy products |
| Portion Size Inflation | Restaurant portions increased 138% since 1970s |
| Urban Sprawl | Each additional hour of car commuting increases obesity risk by 6% |
| Food Deserts | 23.5 million Americans lack access to affordable fresh foods |
| Screen Time | Each daily screen hour increases childhood obesity risk by 12% |
| Ultra-Processed Foods | Now constitute 58% of calorie intake in developed nations |
| Reduced Physical Labor | Daily calorie expenditure dropped 120-140 calories since 1960s |
| Sleep Disruption | Inadequate sleep alters hunger hormones, increasing obesity risk by 55% |
4. Lifestyle Diseases and Hypertension: Living at Permanent Speed
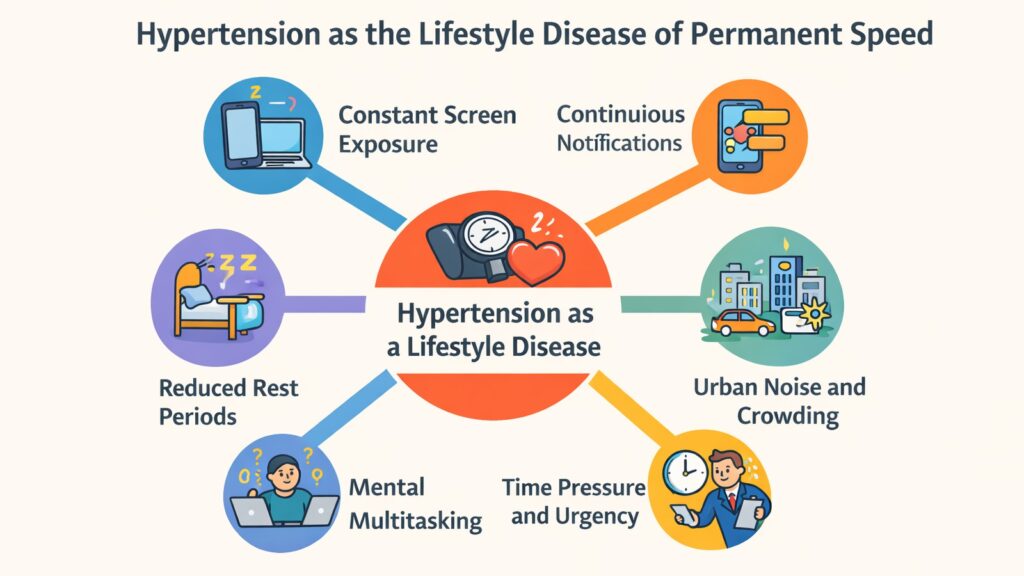
Silence defines hypertension. Most people with elevated blood pressure feel nothing unusual. No pain signals the problem. No obvious symptoms demand attention. Yet inside, pressure builds against arterial walls with every heartbeat, causing microscopic damage that accumulates over the years. This makes hypertension one of the most dangerous lifestyle diseases, earning its nickname as the silent killer. By the time complications appear, organs have already suffered irreversible harm.
Modern life operates at a pace unimaginable to previous generations. Constant connectivity means constant availability. Phones buzz with notifications. Emails demand immediate responses. News cycles deliver an endless stream of urgency and alarm. The mind rarely rests. This perpetual stimulation keeps the nervous system in a heightened state. Blood pressure, which should fluctuate naturally throughout the day, remains elevated. The body cannot distinguish between actual threats and the abstract stressors of modern existence.
Digital overload plays a significant role. Screens dominate waking hours, from morning phone checks to evening television. Blue light disrupts sleep patterns. Social media triggers comparison and anxiety. The dopamine loops of apps and games create addictive cycles. Each notification provides a small hit of stress hormones. Multiply this by dozens or hundreds of daily interruptions, and the cumulative effect becomes clear. The nervous system, designed for occasional acute stress, faces chronic low-level activation that never fully resolves.
Time pressure compounds the problem. Schedules pack tighter. Multitasking becomes necessary. The concept of doing nothing feels uncomfortable or guilty. People rush through meals, skip breaks, and sacrifice sleep. This constant hurry translates into sustained physiological activation. Heart rate stays elevated. Blood vessels constrict. Stress hormones circulate continuously. Over time, this becomes the new normal, the baseline the body adapts to. Hypertension develops not from dramatic events but from the accumulated weight of living at permanent speed, making it emblematic of how lifestyle diseases emerge from the structure of daily existence.
Modern Triggers of Hypertension Among Lifestyle Diseases
| Lifestyle Trigger | Effect on Blood Pressure |
|---|---|
| Chronic Stress | Sustained cortisol elevation increases systolic pressure 10-15 mmHg |
| Excessive Salt Intake | High sodium diets raise blood pressure by 5-10 mmHg on average |
| Physical Inactivity | Sedentary individuals face 30% higher hypertension risk |
| Alcohol Consumption | More than 3 drinks daily increases systolic pressure by 3-4 mmHg |
| Obesity | Excess weight accounts for 65-75% of primary hypertension cases |
| Sleep Deprivation | Each hour of lost sleep increases hypertension risk by 37% |
| Digital Overstimulation | Constant notifications maintain sympathetic nervous system activation |
| Noise Pollution | Chronic noise exposure increases blood pressure by 1-2 mmHg per 10 dB |
5. Lifestyle Diseases and Chronic Respiratory Conditions: Breathing Modern Air
Smoking receives most attention when discussing respiratory disease. This focus, while important, obscures a larger reality. Chronic respiratory conditions have become lifestyle diseases shaped by environmental exposures that affect everyone, smokers and non-smokers alike. Urban air quality, indoor pollution, occupational hazards, and daily environmental factors contribute to lung damage that accumulates silently over decades. The air people breathe carries more than oxygen. It carries the consequences of how societies organize space, production, and transportation.
Cities concentrate pollutants. Traffic generates particulate matter and nitrogen oxides. Industrial facilities release chemical compounds. Construction dust becomes airborne. These pollutants are small enough to penetrate deep into lung tissue, causing inflammation and scarring. The effects are dose-dependent and cumulative. Each breath in a polluted environment adds to the total burden. Children growing up in high-pollution areas show reduced lung capacity compared to those in cleaner environments. By adulthood, the damage is measurable and often irreversible.
Indoor air quality represents an overlooked dimension of respiratory lifestyle diseases. People spend roughly 90 percent of their time indoors, where air can be more polluted than outside. Building materials off-gas chemicals. Cleaning products release volatile compounds. Poor ventilation traps pollutants. Mold grows in damp environments. Gas stoves release nitrogen dioxide at concentrations that would be prohibited in outdoor environments. Home becomes a chronic exposure site, particularly for children, elderly people, and those working from home. The lungs, designed to filter occasional irritants, face constant challenge.
Occupational exposures affect millions. Construction workers inhale dust and silica. Healthcare workers encounter infectious aerosols and chemical disinfectants. Agricultural workers breathe pesticides and organic particles. Office workers face poor ventilation and recycled air. Many occupations involve respiratory hazards that go unrecognized until disease appears. Chronic obstructive pulmonary disease, asthma, and pulmonary fibrosis often develop not from single acute exposures but from years of cumulative damage. Among lifestyle diseases, respiratory conditions demonstrate how environmental design shapes health outcomes across entire populations.
Lifestyle and Environmental Factors in Chronic Respiratory Diseases
| Factor | Respiratory Impact |
|---|---|
| Urban Air Pollution | Long-term exposure reduces lung function by 3-5% per decade |
| Traffic Emissions | Living near major roads increases asthma risk by 25-50% |
| Indoor Pollutants | Poor indoor air quality contributes to 3.8 million deaths annually |
| Occupational Exposures | Workplace hazards account for 15% of chronic lung disease cases |
| Secondhand Smoke | Increases lung disease risk by 20-30% even without direct smoking |
| Physical Inactivity | Sedentary lifestyle reduces respiratory muscle strength and lung capacity |
| Childhood Exposures | Early pollution exposure increases lifelong respiratory disease risk |
| Climate Change | Rising temperatures increase air pollution and allergen levels |
6. Lifestyle Diseases and Fatty Liver Disease: Damage Without Alcohol
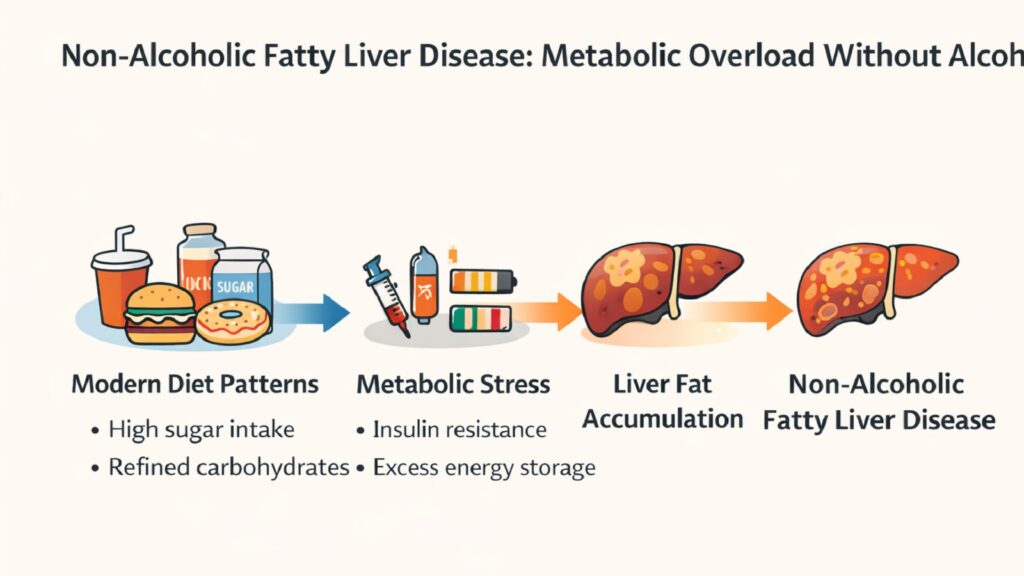
Non-alcoholic fatty liver disease represents one of the most surprising and rapidly growing lifestyle diseases. The liver, a resilient organ capable of remarkable regeneration, faces a new kind of assault. Not from alcohol, as the name makes clear, but from sugar, refined carbohydrates, and sedentary living. Many people develop serious liver damage without ever suspecting a problem. The disease progresses silently, often discovered only through routine blood work or imaging performed for other reasons.
The mechanism involves metabolic overload. When people consume more energy than they burn, the body must store the excess. Some goes to fat tissue under the skin. But the liver also begins accumulating fat droplets within its cells. This process, called hepatic steatosis, represents the first stage of fatty liver disease. In many cases, it causes no symptoms and requires no immediate treatment. But in a significant percentage of people, inflammation develops. The fat-laden liver becomes inflamed, progressing to non-alcoholic steatohepatitis. From there, the path can lead to fibrosis, cirrhosis, and liver failure.
Sugar consumption plays a central role. Fructose, abundant in sweetened beverages and processed foods, gets metabolized primarily in the liver. Unlike glucose, which cells throughout the body can use directly, fructose must be processed centrally. High intake overwhelms the liver’s capacity, forcing conversion to fat. This fat accumulates locally rather than being distributed to other tissues. The modern diet, heavy in added sugars and refined carbohydrates, creates constant pressure on this metabolic pathway. The liver, evolved to handle occasional sweet foods like fruit, faces daily overload from soda, candy, and sweetened products.
Physical inactivity compounds the problem. Exercise helps the body burn stored energy and improves insulin sensitivity. Without regular activity, glucose regulation deteriorates. The liver receives signals to store more energy even when it is already overloaded. Visceral fat accumulates around internal organs, releasing inflammatory compounds that further damage hepatic tissue. Non-alcoholic fatty liver disease often clusters with other lifestyle diseases like obesity, diabetes, and cardiovascular disorders, forming a syndrome of metabolic dysfunction. The liver silently bears the cost of modern dietary patterns and sedentary living.
Lifestyle Contributors to Fatty Liver Disease
| Factor | Impact on Liver Health |
|---|---|
| Added Sugar Intake | High fructose consumption increases fatty liver risk by 55% |
| Refined Carbohydrates | White bread and pasta diets triple fatty liver disease likelihood |
| Sedentary Behavior | Physical inactivity doubles progression from simple steatosis to inflammation |
| Obesity | Present in 75% of fatty liver disease cases, central obesity particularly harmful |
| Metabolic Syndrome | Insulin resistance accelerates fat accumulation in hepatic tissue |
| Ultra-Processed Foods | High consumption associated with 25% increased disease prevalence |
| Soft Drink Consumption | Daily sugary beverage intake increases risk by 60-70% |
| Rapid Weight Gain | Quick increases in body weight overwhelm liver’s metabolic capacity |
7. Lifestyle Diseases and Mental Health Disorders: The Weight of Modern Life
Depression and anxiety have traditionally been understood as psychiatric conditions, rooted in brain chemistry or traumatic experiences. This framing is not wrong but incomplete. Mental health disorders increasingly emerge as lifestyle diseases, shaped profoundly by how modern life is structured. Social isolation, constant comparison, disrupted sleep, cognitive overload, and performance pressure create an environment that exhausts mental resilience. The mind, like the body, responds to cumulative stress with breakdown.
Digital technology has transformed social connections. People maintain hundreds of online contacts while feeling profoundly alone. Social media platforms present curated versions of others’ lives, fostering endless comparison. The dopamine hits from likes and comments create addictive patterns that replace deeper engagement. Real-world communities have weakened as digital interaction has grown. People move more frequently for work, losing stable social networks. Extended families live far apart. Neighborhoods lack the informal gathering spaces that once facilitated connection. This isolation weighs heavily on mental health, especially for young people forming their sense of self in an age of algorithmic recommendations and virtual performance.
Sleep disruption compounds the problem. Electronic devices emit blue light that suppresses melatonin production. Entertainment and work extend late into the night. The boundary between day and night blurs. Many people exist in a state of chronic sleep debt, getting by on insufficient rest night after night. Sleep is when the brain consolidates memories, processes emotions, and clears metabolic waste. Without adequate sleep, emotional regulation deteriorates. Anxiety increases. Depressive symptoms worsen. The relationship is bidirectional, with poor sleep contributing to mental health problems and mental health problems disrupting sleep.
Performance pressure pervades modern life. Academic achievement determines life trajectories from early childhood. Career advancement requires constant skill development. Financial stability feels precarious. The gap between effort and reward seems to widen. People work longer hours for less security. The sense of control over one’s future diminishes. This chronic uncertainty and pressure take a psychological toll. Among lifestyle diseases, mental health disorders reveal how deeply the environment shapes internal experience. The mind does not exist in isolation but responds to the social, physical, and temporal structures within which life unfolds.
Lifestyle Factors Shaping Mental Health as a Lifestyle Disease
| Factor | Mental Health Impact |
|---|---|
| Social Isolation | Increases depression risk by 50% and anxiety disorders by 40% |
| Social Media Use | More than 3 hours daily increases mental health risks by 60% |
| Sleep Deprivation | Less than 6 hours nightly increases depression likelihood by 80% |
| Physical Inactivity | Sedentary lifestyle increases depression risk by 25-30% |
| Work Stress | Job strain doubles the risk of major depressive episodes |
| Urban Living | City residents show 21% higher anxiety disorder rates than rural areas |
| Screen Time | Excessive digital use correlates with 35% higher psychological distress |
| Loss of Community | Weak social ties increase mental health disorder risk by 45% |
8. Lifestyle Diseases and Cancer Risk: The Long-Term Accumulation Effect
Cancer feels random and arbitrary. A cell mutates. Growth spirals out of control. Tumors form. But while chance plays a role, lifestyle factors exert substantial influence over cancer risk. Certain cancers are linked directly to long-term lifestyle patterns, making them classifiable among lifestyle diseases. Diet, physical activity, body weight, sleep, and chronic inflammation shape the cellular environment over decades. Each factor alone may have modest effects. Combined and sustained over years, they significantly alter cancer probability.
Diet affects cancer risk through multiple pathways. Processed meats contain compounds that damage DNA and promote tumor growth. Diets low in fiber allow carcinogens to contact intestinal walls longer. Excess calorie intake drives cellular proliferation. Conversely, diets rich in vegetables, fruits, and whole foods provide protective compounds. The difference becomes apparent only over decades. No single meal causes cancer. But years of processed food consumption versus whole food eating create divergent risk profiles.
Physical inactivity increases cancer risk through several mechanisms. Exercise regulates hormones like insulin and estrogen that influence cell growth. It reduces inflammation throughout the body. It helps maintain a healthy body weight. Active people show lower rates of colon, breast, and endometrial cancers. The protection is dose-dependent. More activity provides more benefit. Yet modern life makes sustained movement difficult. Jobs require sitting. Transportation is passive. Recreation is often sedentary. The body’s defense systems, which evolved with constant physical activity, operate in a state of relative disuse.
Sleep disruption affects cancer risk in ways researchers are still mapping. During sleep, the body repairs DNA damage and regulates immune function. Chronic sleep deprivation weakens these processes. Shift workers show elevated cancer rates, particularly breast and prostate cancers. The disruption of circadian rhythms seems to play a role. Artificial light at night suppresses melatonin, a hormone with anti-cancer properties. Modern life extends waking hours artificially, using electric lighting to push back darkness. The biological rhythms shaped by millions of years of evolution face constant disruption.
Chronic inflammation links many lifestyle diseases to cancer. Obesity creates low-grade inflammation throughout the body. Inflammatory compounds released by fat tissue can damage DNA and promote tumor growth. Smoking causes inflammation in lung tissue. Alcohol inflames the digestive tract. Poor diet, physical inactivity, and stress all contribute to inflammatory states. Over decades, this chronic inflammation creates conditions favorable to cancer development. Lifestyle-linked cancers represent the accumulated cellular damage from years of environmental exposure and behavioral patterns. They demonstrate how daily choices, repeated over time, shape biological outcomes at the deepest level.
Lifestyle Factors in Cancer Development Among Lifestyle Diseases
| Factor | Cancer Risk Impact |
|---|---|
| Obesity | Increases risk for 13 types of cancer, accounting for 7-8% of cases |
| Physical Inactivity | Lack of exercise contributes to 16-19% of colon cancer cases |
| Poor Diet | Unhealthy eating patterns linked to 30-35% of cancer deaths |
| Alcohol Consumption | Accounts for approximately 5-6% of cancer cases and deaths globally |
| Tobacco Use | Responsible for 22% of cancer deaths worldwide |
| Sleep Disruption | Chronic sleep debt increases cancer risk by 20-30% in some studies |
| Chronic Inflammation | Persistent inflammatory states contribute to 15-20% of cancer cases |
| Environmental Exposures | Pollution and chemical exposures account for 8-10% of cancers |
Conclusion: Lifestyle Diseases and the Future of Global Health Resilience
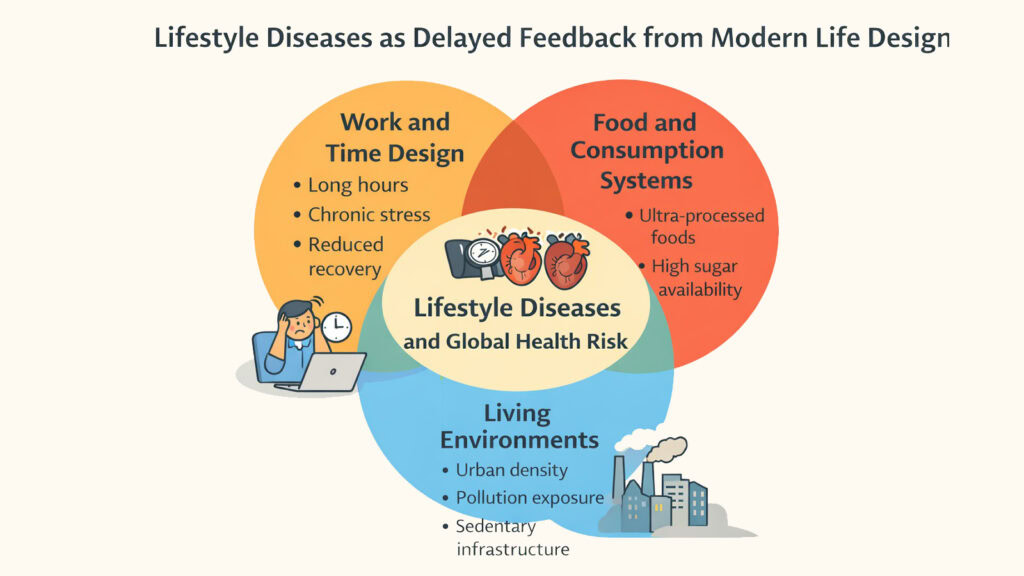
The eight lifestyle diseases examined here share a common architecture. They emerge not from random misfortune but from how modern societies structure daily existence. Work that demands sitting for hours. Food systems that prioritize profit over nutrition. Cities are designed for cars rather than people. Technology that fragments attention and disrupts sleep. Social environments that isolate while claiming to connect. Each element seems minor in isolation. Together, they create conditions that systematically undermine human health.
What makes lifestyle diseases particularly challenging is their delayed feedback. Unlike infectious diseases that strike quickly, lifestyle diseases develop over years or decades. By the time symptoms appear, damage has often progressed substantially. The liver shows scarring. Arteries have narrowed. Beta cells have failed. Mental resilience has eroded. This lag between cause and effect makes prevention difficult. People lack immediate signals that their daily patterns are harmful. The consequences arrive too late to be easily reversed.
Yet this delay also represents an opportunity. Lifestyle diseases, unlike genetic conditions or infectious outbreaks, are largely preventable. Small changes, sustained over time, can significantly alter trajectories—resulting in more movement in daily routines. Better food environments. Work cultures that respect rest. Cities designed for walking. Digital habits that preserve attention and sleep. None of these changes happens quickly or easily. They require rethinking systems rather than just individual behavior. But the potential for prevention is real.
The future of global health depends on recognizing lifestyle diseases as systemic challenges rather than individual failings. Medical treatment alone cannot solve problems rooted in environmental design and social structure. Pills can manage blood sugar, but cannot fix food systems. Surgery can bypass clogged arteries, but it cannot reduce chronic stress. Mental health medications can stabilize mood, but cannot rebuild community. Addressing lifestyle diseases requires looking upstream, examining the conditions that produce ill health in the first place.
This is not a call for personal perfection or ascetic living. Nor is it about returning to some imagined past. The goal is designing modern life in ways that support rather than undermine health. Making the healthy choice the easy choice through environmental design. Creating work cultures that value human sustainability. Building cities where movement happens naturally. Regulating food systems to prioritize public health. These changes seem difficult because they challenge powerful economic interests and established patterns. But they become necessary once the full cost of lifestyle diseases becomes clear. The burden on healthcare systems is growing unsustainable. Productivity suffers as populations sicken. Quality of life diminishes for millions.
Global health resilience in the coming decades will depend on confronting this reality honestly. Lifestyle diseases are not inevitable. They result from specific choices about how societies organize themselves. Different choices would produce different outcomes. The eight diseases explored here, from diabetes to cancer, represent different expressions of the same underlying pattern. They are the price of abundance without wisdom, comfort without consideration, speed without rest. Recognizing them as such opens pathways toward genuine prevention, not just better treatment. The challenge is not medical but social, not individual but collective. And that, perhaps, is where hope lies.
Preventive Approaches to Major Lifestyle Diseases
| Lifestyle Disease | Key Prevention Strategy |
|---|---|
| Type 2 Diabetes | Regular physical activity and whole food diets reduce risk by 58% |
| Cardiovascular Diseases | Stress management, adequate sleep, and movement prevent 80% of cases |
| Obesity | Environmental redesign for walkability and healthy food access |
| Hypertension | Sodium reduction and stress reduction lower blood pressure effectively |
| Chronic Respiratory Diseases | Air quality improvement and smoke-free environments protect lung health |
| Non-Alcoholic Fatty Liver Disease | Reduced sugar intake and regular exercise reverse early-stage disease |
| Depression and Anxiety Disorders | Community connection, physical activity, and sleep hygiene improve outcomes |
| Lifestyle-Linked Cancers | Healthy weight maintenance and plant-rich diets reduce risk significantly |
Read More Science and Space Articles
- Peaches: 6 Fascinating Secrets of Genetic Evolution
- Cherries Reveal 6 Powerful Secrets of Their Red Glow
- Pears Reveal 6 Amazing Secrets of Genetic Evolution
- 8 Amazing Ways Living Organisms Turn Chemistry Into Life
- Origin of Life: 8 Stunning Theories That Spark Curiosity
- Apples Boost Gut Health: 6 Brilliant Benefits Revealed
- 8 Amazing Fruit Families With Their Nutrition Secrets
- 8 Incredible Rosaceae Fruits With Phytochemical Power
- Pinot Noir Grapes: 6 Stunning Anatomy Secrets Revealed
- Vitaceae Fruits: 8 Delightful Grapes That Wow Your Senses